Tumors Under Physical Stress Inside the Body May Not Respond as Well to Chemotherapy
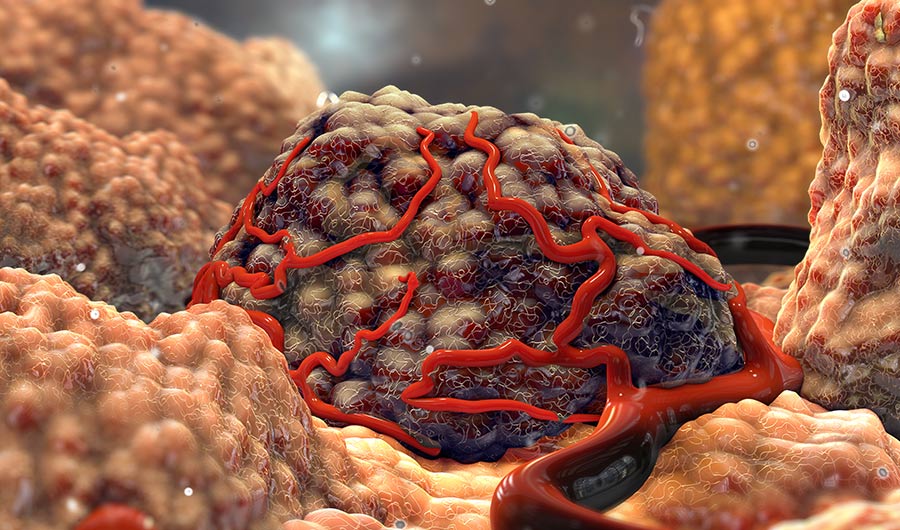
Nathan Devery via Shutterstock
(Inside Science) -- Scientists have long known that the biochemical environment around living cells can encourage or suppress their growth. More recently, researchers have begun recognizing that mechanical cues such as pushing or stretching may be equally important.
Now, researchers have found that cancer cells that are compressed by other tissue may not respond as well to chemotherapy drugs. Their in vitro experiments on model tumors point to a possible strategy for treatment that alleviates compressive stress experienced by cancer cells, which may then boost the effects of chemotherapy. The study was published online Friday in the journal Physical Review Letters.
"Mechanical stress is increasingly recognized to be important for cancer, and clinicians are only just starting to account for this," said study author Morgan Delarue, a biophysicist at the French National Centre for Scientific Research. "Our results suggest that, when designing new therapies, we should also account for their effects on a tumor’s mechanical environment."
Cancer cells live in a diverse, bustling neighborhood made up of connective tissue cells, immune cells, blood cells, collagen, enzymes and proteins. This so-called microenvironment around the tumor plays a crucial role in the development and progression of cancer. In addition to biochemical signals from the microenvironment, physical signals such as changes in tissue stiffness or pressure can drive tumor growth and metastasis.
Delarue and his colleagues work with tumor spheroids -- basically, balls of cancer cells grown in a culture medium that mimic real tumors in the lab. Previously, they demonstrated that compressing tumor spheroids inhibits their growth rate. That’s because as a solid tumor grows within a limited space, it has to push harder against its surrounding environment, making it unable to grow or spread as quickly.
The current study explores the relationship between compressive stress and chemotherapy. One of the biggest challenges in cancer therapy is drug resistance, where a given chemotherapy or other medication no longer works for a patient, even in cases where it once did. Increased drug resistance means the loss of viable treatment options, leaving patients vulnerable to disease recurrence and death.
"Our question was, would mechanical stress lower the efficacy of a given chemotherapeutic by decreasing the amount of target cells?" said Delarue. Chemotherapy specifically targets cells that are growing and dividing, so he wondered what the effects of growth-inhibiting compression would be on such a drug.
The researchers attempted to find the answer by compressing tumor spheroids made of pancreatic cancer cells and adding gemcitabine, a chemotherapy medication. The spheroids were embedded and confined within a polymer solid as a way to introduce growth-induced pressure. While the unconfined spheroids decreased in size by roughly 30% to 40% when treated with gemcitabine, their confined counterparts shrank by only 10%.
Delarue and his colleagues came up with two possible explanations for this result. One is that compressive stress triggers a series of chemical signals inside the cell that inhibits the drug directly. The other hypothesis involves a more indirect route, where compression of the tumor leads to a decrease in tumor growth rate, which in turn would make chemotherapy less effective.
When these assumptions were incorporated into a mathematical model, the second mechanism correctly predicted the experimental data. This result suggests a novel mechanical form of drug resistance may arise from compressive stress. Cancer cells sense pressure and release signals to stop tumor growth, and the lack of growing cells leave chemotherapy with nothing to target.
Delarue suggests a possible strategy to overcome chemotherapy resistance would be to give patients a drug that reduces compressive stress in order to trigger cancer cells to grow and divide again. He acknowledges the counterintuitive nature of this method, but if tumor growth is carefully timed and controlled, it could allow chemotherapy to eradicate the tumor once and for all.
"This is a very interesting study showing in vitro that mechanical compression of cancer cells can cause resistance to chemotherapy," said Triantafyllos Stylianopoulos, a biophysicist at the University of Cyprus who was not involved in the research. "Tumor microenvironment targeting with the aim to alleviate mechanical forces in tumors is promising, and this study nicely supports this concept, providing another argument in favor of it."
However, putting the idea of drugs that reduce stress on tumors into practice has proved less straightforward. Animal studies in which chemotherapy was combined with hyaluronidase, an enzyme that alleviates compressive forces in the tumor microenvironment, looked promising. But in 2019, a clinical trial in human patients with metastatic pancreatic cancer failed to demonstrate an improvement in overall survival, and Halozyme Therapeutics halted drug development as a result.
Stylianopoulos believes that in order to be effective, mechano-therapeutic drugs must address both the tumor's mechanical properties and its microenvironment. Losartan, a drug originally used to treat hypertension, has shown some promise in these areas.
John D. Martin, head of research at nanotechnology company NanoCarrier, agreed that the results support the incorporation of mechanical stress as a factor when developing new therapies for cancer. Martin and his colleagues recently published a study on dexamethasone, a drug with anti-inflammatory properties, showing that it reduces tissue stiffness and solid stress in the tumor microenvironment.
"This work provides evidence of an additional rationale for using solid stress-alleviating therapies such as losartan and dexamethasone in combination with chemotherapy," said Martin, who was also not involved with the study. "Solid stress-alleviating therapies combined with chemoradiation are already advancing in clinical trials, and these findings support this course."

